As our emergency triage monitoring system moves from development into testing, one of the most critical phases has been the validation of the complete pipeline — from wearable data acquisition, through edge processing, all the way to visualization in our app interface. This step is vital not only to confirm that the system technically works, but also to assess its reliability, responsiveness, and clinical relevance.
End-to-End System Integration: From Sensor to App
To simulate a real deployment scenario, we set up the entire infrastructure:
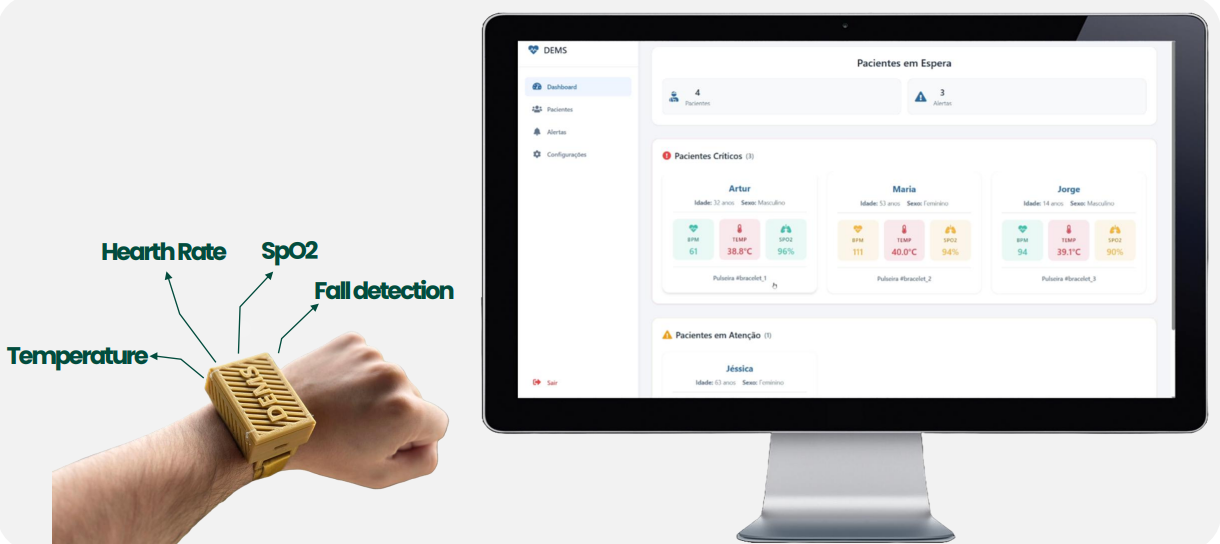
- Wearable device: Our prototype is fully equipped with multiple sensors as we explained in previous posts, collecting continuous physiological data.
- Edge gateway: A Laptop that serves as the data receiver and TCP/IP server.
- Local server (laptop): Collects sensor readings, processes them into .csv files, and uses a Python application to ingest and structure the data.
- MongoDB database: Stores this processed data to make it accessible and persistent.
- Web-based app: Hosted on the same laptop, the application fetches the stored data and displays it in a clean, real-time dashboard.
We tested the system using a tablet connected to the same Wi-Fi network as the laptop. Since the server and app are hosted locally, any device on the same network can access the dashboard through a browser. This demonstrates an important feature of architecture scalability and device independence — making it suitable for deployment in real hospital environments.
Sensor Validation: What Works and What Needs Attention
Sensor validation is central to our system’s credibility. For this, we compared our sensor readings with trusted commercial or clinical devices, including:
- A thermometer (for temperature comparison with the MLX90614 infrared sensor)
- A smartwatch (to validate the MAX30102 heart rate and SpO₂ values)
- A standard cuff-based blood pressure monitor
Individually, the sensors performed within ranges. We observed consistent readings that closely matched the reference devices acceptable, confirming their potential for medical monitoring in controlled settings.
However, some challenges emerged:
MAX30102 – Accurate but Highly Sensitive
While the MAX30102 is known for its precision in ideal conditions (especially when used on fingertips), its accuracy dropped significantly when integrated into our wrist-worn bracelet format. This is due to several physiological and mechanical factors:
- Lower blood flow in the wrist compared to fingertips
- Movement artifacts when worn loosely or during patient motion
- Reduced skin contact, leading to unreliable SpO₂ and heart rate readings
Although the sensor performed well in static tests, this limitation may affect real-time triage assessments. As a result, we’re exploring some solutions to this problem, such as improved mechanical housing for better contact, and signal-processing techniques to stabilize readings.
MLX90614 – A Contactless Advantage
The infrared MLX90614 temperature sensor proved much more robust, providing consistent and reliable values. Its non-contact nature makes it especially suited for hospital use, where hygiene and speed are essential.
System Performance & Responsiveness
Our goal was not only to validate sensor accuracy, but also to test the real-time data pipeline. During these trials, we confirmed that:
- Data was received by the server without loss or duplication
- The Python app correctly processed and cleaned the raw data
- The MongoDB database stored the structured data as intended
- The web interface displayed information with low latency and frequent updates
The system performed stably over extended periods, demonstrating reliability and low response time — even with multiple data streams. Importantly, this setup confirmed that multiple devices (e.g., a nurse’s tablet, a doctor’s phone or computer in the hospital office) can access the monitoring interface simultaneously, simply by being on the same network. This aligns with our vision for a distributed, scalable emergency monitoring system.
What This Validation Taught Us
The tests performed were essential for identifying strengths and weaknesses:
- Strengths: Functional architecture, responsive app, reliable temperature data, clean database integration.
- Weaknesses: Sensor calibration, sensitivity to movement, and the need for mechanical improvements to improve wearability and reading consistency.
These insights will inform the next design iteration, helping us refine both the hardware layout and signal processing logic, and ultimately move closer to a robust and medically dependable solution. Until the presentation day, the improvement of the readings, and fixing some bugs/adding some features on the app (and the system itself) we’ll be our main focus.
Conclusion
Validation is more than ticking off a checklist — it’s a process of discovering limitations and optimizing real-world performance. This stage has confirmed that our system — from sensors to app — is functional, insightful, and well-aligned with its use case in emergency triage. We still have challenges to solve, particularly in wearable integration, but this step marks a critical milestone in transforming a promising idea into a viable healthcare tool.